Dry eye therapeutics today
Focusing on dry eye disease (DED), the third Ocular Therapeutics Evening (OTE) finally went ahead after a five-month wait. It’s been a while since we had an in-person meeting, so it was great to see at least the top halves of some familiar faces again! It was also entertaining to see the Covid tracer app used to scan the QR code for CPD points.
From blinking to blood
Professor Jennifer Craig from the University of Auckland’s Ocular Surface Laboratory (OSL) led proceedings, sharing some recent research showing that young Asian adults exhibit more blink incompleteness, meibomian gland (MG) dropout, corneal staining and lid wiper epitheliopathy, despite no differences in DED symptoms and tear film characteristics. Research shows the ethnic disparity in MG dropout becomes greater with age, thus more Asians suffer with DED symptoms later in life. Prof Craig encouraged optometrists to prescribe blink exercises and advise patients to use blink-reminder apps such as EyeLeo, because incomplete blinking may predispose patients, particularly Asians, to the development of evaporative dry eye.

Prof Jennifer Craig
Re:Vision’s Dr Trevor Grey focused on the use of serum drops for severe ocular surface diseases. Serum from blood contains several growth factors, neuropeptides and vitamins, which are also present in a healthy tear film. Drops composed of 25% serum and 75% saline are suitable for patients who are unresponsive to other dry eye treatments, especially those with Sjogren’s syndrome, persistent epithelial defect, neurotrophic ulcers, chemical and thermal burns, as well as inherited conditions causing limbal stem cell deficiency. The serum drops are manufactured from the patient’s blood and this blood bank service comes at no extra cost. Those who cannot donate blood – such as patients who are immune-compromised or receiving cytotoxic treatments – can obtain serum drops from other donors. Each requires ophthalmic prescription and comes in a three-month supply, with the patient donating blood every six months.
Dr Trevor Gray
Challenging external DED causes
OSL’s Dr Alex Müntz discussed the impact of digital devices on DED and younger people. Children today are exposed to extended screen use, which not only contributes to myopia and DED, said Dr Müntz, but also impacts their educational outcomes, sleep patterns and mental and physical health. New Zealand has one of the highest uses of digital devices in schools, yet productivity has been dropping. To manage DED in children, it is important to educate them and their parents about appropriate screen use. Some useful reminders include maintaining good reading distance and posture, taking regular breaks, positioning the computer screen below eye level and increasing humidity in the working environment.

Dr Alex Müntz
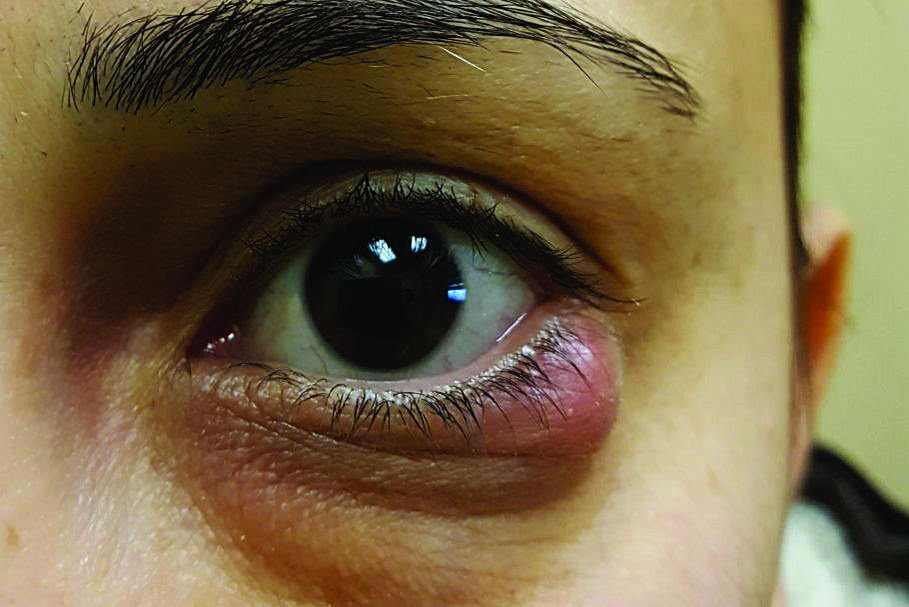
Eye Institute’s Dr Jay Meyer then tackled iatrogenic dry eye*, which is commonly caused by systemic medications such as antihistamines, anti-depressants, anti-hypertensives, diabetic medication, anti-cancer agents, hormone replacement therapy, anti-androgen therapy, vitamin A analogue Accutane (used to treat severe acne and prevent some forms of skin cancer) and monoclonal antibodies. As eyecare practitioners, we should educate patients about systemic medications and how they can contribute to dry eyes and encourage them to discuss this with their GPs to see if any non-essential systemic medications can be reduced. Of course, topical medications such as glaucoma drops can also cause dry eye, largely due the cytotoxic effects of preservative benzalkonium chloride (BAK). Dr Meyer’s advice was to stop the medication contributing to dry eye, if possible, and switch to preservative-free medications (or ones with lower-toxicity preservatives), use a new medication that has a different mechanism of action and use preservative-free lubricants to alleviate symptoms.

Dr Jay Meyer
Wrapping up the evening, Dr Marcy Tong shared some interesting dry eye cases encountered at the university’s Grafton optometry clinic. It was fascinating to see the transformation of patients’ dry eye symptoms and attitudes from unhappy and noncompliant to compliant and creative with home treatment and improved quality of life. It is key to coach patients that dry eye is a long-term management issue and not a one-time magic cure, she said, and to incorporate treatment routines with patients’ lifestyles to increase compliance. Dr Tong tells patients that cleaning their eyelids is just like brushing teeth – leave the lid cleaner next to the toothbrush and use it twice a day, otherwise the bacteria will build up again. We also heard about one patient who made her own single-eye wheat bag so she could continue to work while applying a hot compress, while another purchased his own Mastrota meibomian paddle and had to be advised not to use it due to the risk of corneal abrasion!
* https://eyeonoptics.co.nz/articles/archive/iatrogenic-ded-do-ecps-cause-ded/

Charisse Kuo is a therapeutically qualified optometrist in the third year of her PhD at the University of Auckland. Her research involves the development of tissue culture models using human donor retinas and choroids to explore the mechanisms behind sight-threatening diseases.