The effect of eye spray phospholipid concentration on tear film and ocular comfort
Dry eye disease (DED) can be described as aqueous-deficient and/or evaporative dry eye1, the latter being more common (78%)2. The lipid layer of tears plays an important role in inhibiting tear film evaporation and in spreading the tears across the ocular surface3. This lipid layer stabilises the tear film, providing a surface tension decrease and 90-95% reduction in aqueous evaporation4.
Phospholipid liposomal sprays are intended to improve the polar properties of the lipid layer, enhancing lipid spread5,6,7. The sprays are applied to closed eyelids and deliver phospholipid liposomes (phosphatidylcholine) to the eyelid margins, where they migrate across the margins7, mixing with the existing lipid reservoir from the meibomian glands upon blinking.
With the availability of newer products containing different concentrations of phospholipids, contradictory outcomes have been reported on the effectiveness of liposomal sprays. Hence, this crossover study compared the effectiveness of a high-concentration phospholipid spray (HCPS) with a low-concentration phospholipid spray (LCPS) on dry eye symptoms and tear film stability.
Method
Tears Again Sensitive (Optima Pharmaceuticals, Germany) (HCPS) and Ocuvers (Innomedis, Germany) (LCPS) formulations were sprayed onto patients’ closed eyelids from a distance of 10cm. Participants were randomised as to which spray they received bilaterally and a gap of 24-120 hours was allowed between visits to ensure product washout.
Ocular comfort symptoms were tested on a visual analogue scale and with the Ocular Surface Disease Index (OSDI) questionnaire. As a sign of tear film stability, non-invasive tear breakup time (NIBUT) was tested subjectively using a Tearscope Plus with a fine grid insert8, recording a median of three measurements. All tests were performed at baseline, 10 and 30 minutes after spray application.
Thirty participants were recruited to allow comparison with 90% power, based on previously reported NIBUT repeatability, to detect a difference of two seconds8. Wilcoxon signed-rank tests were used to analyse results between lipid sprays and Friedman tests, for analysis between timepoints.
Results
Comfort scores (p=0.003) and NIBUT (p=0.017) significantly increased relative to baseline after application of the HCPS, but not when using the LCPS. When comparing HCPS and LCPS, NIBUT was better for HCPS at both the 10 min (p=0.038) and 30 min (p=0.027) timepoints (Fig 1a). Comfort scores were also significantly better for HCPS at the 10 min (p=0.006) and 30 min (p=0.001) timepoints (Fig 1b).
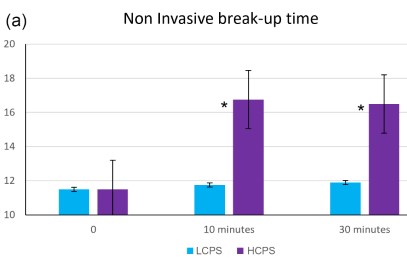
Fig 1a. HCPS significantly outperformed LCPS at the 10 min and 30 min time points in terms of higher NIBUT values (p<0.05)
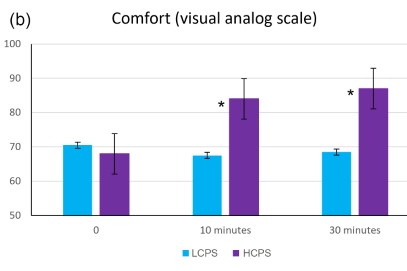
Fig 1b. Superior comfort scores (p<0.05)
Discussion
The use of HCPS resulted in a significant reduction in symptoms and an increase in tear film stability, whereas LCPS did not have any measurable effect. The findings of this study are in accordance with many research groups5,6,7, with some previous studies demonstrating HCPS improves tear film parameters from less than 10 minutes and up to 90 minutes after application5,7.
In DED, increased tear evaporation results in hyperosmolarity, initiating a cascade of inflammatory processes, resulting in epithelial damage, mucin deficiency and reduced wettability of the cornea9. This has been identified as the core mechanism of dry eye9. Any improvement of the lipid layer is a step towards suppressing the vicious cycle, improving the epithelium, mucin layer and consequently the wettability of the cornea4.
This study showed HCPS significantly improved tear film stability and enhanced ocular comfort compared to LCPS. Deficiency of phospholipids prevents the formation of a stable, continuous lipid layer, which, in turn, causes an increased tear evaporation rate10. The improvement of tear film stability after application of the spray with a higher concentration of phosphatidylcholine confirms the positive effect on the tear film. Practitioners should therefore carefully choose an appropriate phospholipid eye spray to maximise the benefit to patients with DED arising from lipid layer deficiency.
References
- Wolffsohn J, Arita R, Chalmers R, et al. TFOS DEWS II Diagnostic Methodology report. Ocul Surf 2017;15:539–574.
- Lemp M, Crews L, Bron A, et al. Distribution of aqueous-deficient and evaporative dry eye in a clinic-based patient cohort: A retrospective study. Cornea 2012;31:472–478.
- Mishima S, Maurice D. The oily layer of the tear film and evaporation from the corneal surface. Exp Eye Res 1961;1:39–45.
- Bron A, de Paiva C, Chauhan S, et al. TFOS DEWS II Pathophysiology report. Ocul Surf 2017;15:438–510.
- Craig J, Purslow C, Murphy P, et al. Effect of a liposomal spray on the pre-ocular tear film. Cont Lens Anterior Eye 2010;33:83–87.
- Dausch D, Lee S, Dausch S, et al. Comparative study of treatment of the dry eye syndrome due to disturbances of the tear film lipid layer with lipid-containing tear substitutes. Klin Monatsbl Augenheilkd 2006;223: 974–983.
- Pult H, Gill F, Riede-Pult B. Effect of three different liposomal eye sprays on ocular comfort and tear film. Cont Lens Anterior Eye 2012;89: E1035–E1041.
- Guillon J. Use of the Tearscope Plus and attachments in the routine examination of the marginal dry eye contact lens patient. Adv Exp Med Biol 1998;438:859–867.
- Craig JP, Nelson JD, Azar DT, et al. TFOS DEWS II report executive summary. Ocul Surf 2017;15:802–812.
- Craig J, Tomlinson A. Importance of the lipid layer in human tear film stability and evaporation. Optom Vis Sci 1997;74:8–13.
Adapted from Pult H, Khatum F, Trave-Huarte S, Wolffsohn J (2021). Effect of eye spray phospholipid concentration on the tear film and ocular comfort. Eye & Contact Lens 2021 Aug 1;47(8):445-448.

Dr Sònia Travé Huarte is a postdoctoral researcher and optometrist specialising in dry eye treatment, specialist contact lenses, anterior ocular surface disease management, meibomian gland dysfunction and corneal pain. She is also a clinical supervisor on the optometry programme and gained her PhD from Aston University, UK, supervised by Professors James Wolffsohn and Jennifer Craig.